By Terry Rice
According to a 2010 American Society of Hematology article titled, The Aging Patient with Hemophilia Complications, Comorbidities, and Management Issues, the median life expectancy for persons with hemophilia in the early 20th century was 11 years.
That was my expected lifespan when I was born in 1962. However, with the rapid improvement of hemostatic therapies throughout the 60s and 70s, life expectancy increased to 55-63 years with severe cases on the lower end of this range. By the early 1980s with 73% of people with hemophilia using plasma-derived factor concentrate replacement therapy, life expectancy had increased to nearly 68 years old. Great news for us!
Factor concentrate proliferated through the 1970s, and treatment delays greatly diminished as more and more patients embraced the ease of home infusion, which was quickly becoming the gold standard of care. Then the ominous 1980s were ushered in, and with them, the gains in life expectancy took a sharp drop to an average of 40 years. This, of course, was the result of the HIV and hepatitis C transmission through the very same miracle factor products that initially increased our longevity.
The manufacturing process for clotting factor combined thousands of donations into a single pool from which various therapeutics, including hemophilia factors, were produced. At the time, these processes did not include the same purification and viral inactivation steps currently used to safeguard blood donations.
Hepatitis was known to be a risk for those using factor products. In mid–1981, the CDC began to receive reports of rare illnesses that were soon labeled under the umbrella of acquired immune deficiency syndrome or AIDS, later found to be caused by the HIV retrovirus. The first reports of otherwise healthy hemophiliacs being affected began in mid–1982. And so began the recognition of the blood-borne pathogen that had been spreading through the hemophilia community like wildfire.
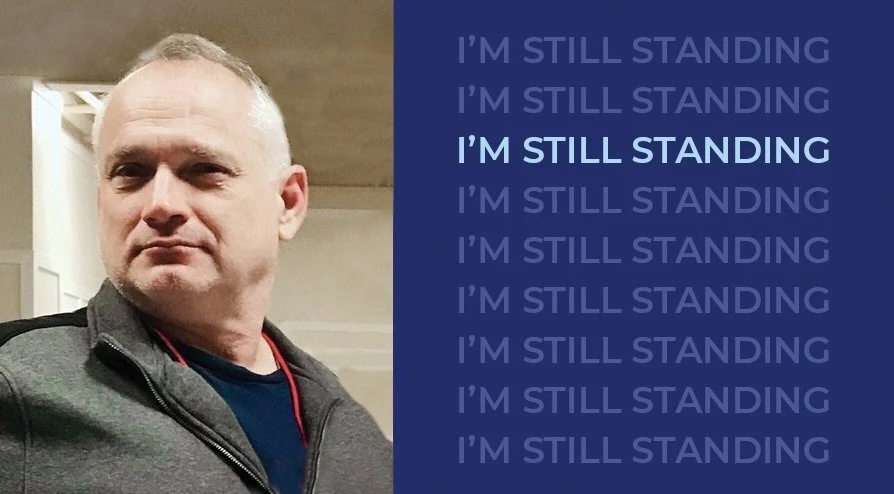
The results of the 1980s are now history. Estimates are that at least 50% of all people with hemophilia and 80% of those with severe disease were lost. I mention this because I am likely the oldest, surviving person with severe hemophilia, HIV, and hep C in my home state of Maine. And I’m only 60 years old.
In 1986, when my HIV diagnosis was confirmed, my doctor told me, “You should really think about what you’re going to do with the time you have left,” which statistically was about 4 or 5 years. This was a sobering reality for someone in their mid-20s. I had worked hard to graduate magna cum laude from college and intended to pursue medical school. But that sobering news and the resulting end of a long-term personal relationship sent me into a spiral of depression.
Dark thoughts occupied my mind for years. I began to drink heavily since there was no reason to preserve my liver. “For what?” I would ask myself! Many of my peers had surrendered their hopes and dreams in life just as I had to adjust to our new reality. Throughout the decades I’ve watched so many friends from my youthful years at camp and clinic visits experience the most traumatic gut-wrenching emotional, physical, and financial assault possible on their humanity. Simply horrible deaths that in part were preventable. The majority of my generation became members of the “Triple H Club” — hemophilia, hepatitis, and HIV. The fact that I survived is remarkable but has carried its own burden and weighed heavy on my mental health.
Those who experience and survive a catastrophic event where most everyone perishes can’t avoid the survivor’s guilt that accompanies one’s escape. Why was I spared this death? It reminds me of a line from the movie, Unforgiven, where just before William Mooney (Clint Eastwood) shoots the sheriff (Gene Hackman), the sheriff says, “I don’t deserve to die this way.” Mooney replies, “Deserves got nothin’ to do with it.” I survived simply by luck of the genetic draw. It’s true that “deserving” had nothing to do with it, but it still has taken an explicit toll on my spiritual and psychological wellbeing.
As years passed and I outlived my doctor’s bleak prognosis, my focus shifted from medicine to real estate and to advocacy. Real estate helped me earn a living, while advocacy allowed me to find and share answers in search of some semblance of accountability for the ‘hemophilia holocaust’, as coined in the early 1990s by the advocacy organization, The Peer Association.
The age demographic existing today reveals the fallout of the 1980s. Comparing the 2000 US Census figures to the 2009 CDC Universal Data Set, 32% of the general population versus just 15% of the hemophilia population was 45 and older. 10% of the general population versus 2% of the hemophilia population was 65 and older, more specifically only 1% with severe disease. Roughly estimated, in 2010 there were approximately 230 severe hemophiliacs 65 or over. That number is not statistically large enough to make conclusions with a high degree of confidence as to what may be unique health challenges for elderly people with hemophilia.
In a way, those of us aging with hemophilia are in uncharted territory. We will likely experience all the same pathologies as those of our non-hemophilia-affected elderly peers, though, I expect some of these health issues will be more acute and have earlier onsets. For example:
We are not immune to and can experience DVTs, strokes and heart attacks. Hemophilia patients will likely need anticoagulants, which may alter how therapies are used.
Joint and muscle damage from previous bleeding episodes, along with natural-aging forms of arthritis and osteoporosis may lead to an increased risk of falls. With intracranial hemorrhage being the third leading cause of death (after HIV and hep C) among those with hemophilia, the risk of falling must be avoided.
Aging people with hemophilia may have an increased risk of developing cancers related to HIV and hep C.
For those with severe factor XIII deficiency, there appears to be an increased incidence of developing inhibitors with advanced age.
Failing eyesight may push aging people with hemophilia to re-evaluate their self-infusion plans and may lead to treating less often.
Hypertension is another emerging concern for aging persons with hemophilia.
At 60, I have now experienced ailments associated with aging such as arthritis (more than just hemolytic arthropathy), hypercholesterolemia, disk degeneration of L3-L4 requiring fusion, fatigue, some imbalance issues, osteopenia, depression, presbyopia, and the real sad malady, cranial alopecia (hair loss!) to name a few.
With all the “medical bullets” sent my way over time, I’m doing relatively well for being part of the 1% of aged persons with severe hemophilia. I take enough pills now to fill one medium size weekly pill container, but I can see an “AM” and a “PM” weekly pill container in my future!
My situation may sound familiar to you if you too are over 60. My medical care now is primarily handled through my internal medicine physician and supplemented by specialists—Hemophilia Treatment Center clinicians, infectious disease doctor, orthopedist, optometrist, and the occasional gastroenterologist and urologist. My hematology team was once the center of my health wheel, but now serves as just one of its spokes.
Being born with hemophilia today is a much safer, healthier, and enlightened time to take on its challenges. As for my fellow geriatric brothers and sisters with hemophilia, you are one of a small group to have made it. For us to eventually mirror the general aging demographic, as a community, we will need to take more responsibility in finding and coordinating from experts outside of the HTCs when appropriate, adhering to prescribed care plans and being tireless advocates. Then, fortunately, just like everyone else, we will grow old and experience the same issues of the aging American—a concept completely unthinkable six decades ago when I was born.
Stay informed on the latest trends in healthcare and specialty pharmacy.
Sign up for our monthly e-newsletter, BioMatrix Abstract.
By giving us your contact information and signing up to receive this content, you'll also be receiving marketing materials by email. You can unsubscribe at any time. We value your privacy. Our mailing list is private and will never be sold or shared with a third party. Review our Privacy Policy here.
References
Philipp, Claire. “Aging Patient with Hemophilia: Complications, Comorbidities, and Management Issues.” American Society of Hematology, 4 Dec. 2010, https://ashpublications.org/hematology/article/2010/1/191/96370/The-Aging-Patient-with-Hemophilia-Complications.