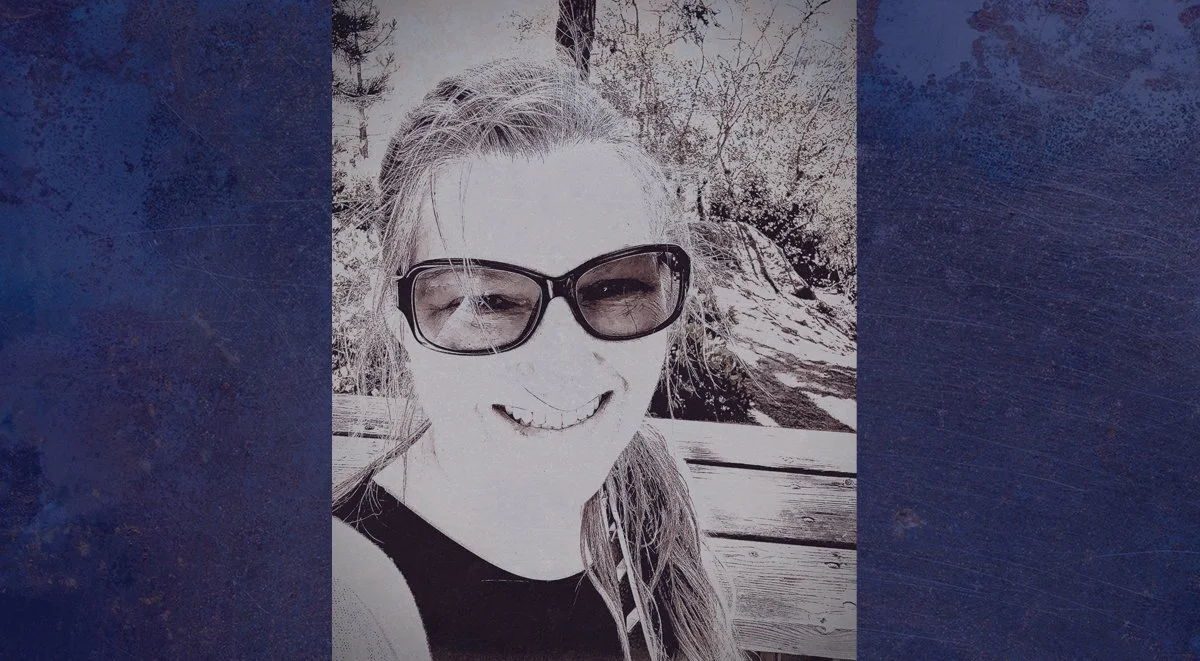
By Ashley Gregory
Anthony and Nicholas were born in 1998, and although I had no family history of bleeding disorders, I now had twins with severe hemophilia A. I became informed about their condition and as they grew, stayed in close contact with our hemophilia treatment center. Also in 1998, NHF launched Project Red Flag, which advocated for women with bleeding disorders. I remember being curious because I had experienced puzzling symptoms throughout my time, but life would take a darker turn, and it would be several years before I could revisit this topic.
One day Anthony didn’t seem right; he was lethargic and not eating. I took him to our pediatrician who suspected the flu. I remember looking directly at her and saying, “Shouldn’t we infuse him since his head is hot, but he has no fever?” She said, “No, just take him home.” Instead, we took him to the emergency room where we learned he had a brain bleed. Despite heroic surgical efforts and finally infusing factor, my son died the next morning – he was only 11 months old. Thus began a slow tumble into despair that our family would not emerge from until well into the next decade.
During subsequent years, researchers were learning that women with the hemophilia gene exhibit unexplained bleeding symptoms and need treatment. Some doctors began successfully working with women to determine how to manage symptoms using factor replacement; they were learning that despite “normal” factor levels, women who experienced unexplained bleeding responded well to factor treatment with no adverse reactions. It was unexplained bleeding that pulled me back into a search for a diagnosis.
While volunteering at my local foundation, I heard women discuss similar untreated symptoms around inexplicable bleeding. It didn’t take long to realize there was a common problem. Women in our community, like me, were experiencing puzzling bleeding that was not addressed despite reporting these symptoms to their doctors. The concerns were usually explained away with comments like, sometimes these things happen, sounds like all the women in your family are like this, or this is just your normal. Were we being ignored, or did the doctors simply not believe us?
This led to a personal investigative journey to seek a diagnosis and treatment while, at the same time, pursuing a career in advocacy and education in bleeding disorders. I began attending local, regional and national programs that provided comprehensive education about my bleeding symptoms and brought me in contact with physicians who were successfully treating women’s bleeding issues using all the medications available to men with bleeding disorders.
I learned about lyonization, which is when one of the two X chromosomes in every cell of a female is inactivated. Lyonization can cause an effective X chromosome to stop working, allowing the other ineffective X chromosome to take over, producing lower factor levels. This led to an even greater understanding of my particular bleeding disorder as a woman with two X chromosomes. Thanks to Dr. Barbara Konkle and the My Life, Our Future genetic analysis project, I learned that some mutations present a high factor level but bleed like a severe! I finally learned that connective tissue disorders can also be present in persons with bleeding disorders, which can then exacerbate bleeding.
Empowered with this knowledge, I confidently entered the HTC near me and presented the information I had gathered, along with my symptoms and history. I trusted I would be heard and cared for. I could not have been more wrong. I even brought my mother along who had been by my side through all my pain and could attest to my history. The treatment center told me my factor levels were too high for my swollen ankles and knees to be caused by hemophilia, and my petechiae were birthmarks.
My unexplained bleeding history was useless in gaining a diagnosis here. I was also seen by the genetics specialist who told me I lacked enough markers to have a connective tissue disorder. I was left with the option to do nothing or to have a synovectomy on my right ankle to see what fluid it contained. Based on my past, I instinctively knew without infusing factor prior to the procedure, the healing process would be long and painful. I declined the surgery in pursuit of a better option.
It was time to try a new approach. I crossed state lines and met with an expert clinician I had met at a national symposium. After a thorough medical evaluation, complete history review of symptoms, physical evaluation and lab workup, I was diagnosed with hemophilia A (symptomatic carrier) and hypermobility syndrome – a connective tissue disorder meaning my joints stretch further than normal. Aminocaproic acid (Amicar®) was prescribed for mucosal bleeding and clotting factor for muscle and joint bleeds. An emergency medical card was prepared with my treater’s name, contact number and diagnosis. A medical alert bracelet was ordered for me, and I was instructed to contact the treatment center and treat on-demand as needed.
Imagine my delight to find when I treated a bleed as my hematologist instructed, my whole body felt better; things that had hurt my entire life stopped hurting; my petechiae cleared, and the swelling in my knees and ankles subsided. Then, as the factor left my body, the pain and baffling bruising would return.
I was able to access treatment from the out-of-state HTC for a short time, and I was emboldened to treat my hemophilia the same way I was as a mother in treating Nicholas’ hemophilia. Since I had been infusing him for years, infusing myself was easy, and I kept a log of bleeds and treatments. I was amazed at the overall improvement in my energy and stamina when using factor!
Moving forward to 2022 – Through my out-of-state HTC, I was able to access free trials of factor products, but those have ended. I am no longer able to have treatment for my bleeds. The system that pays for factor for persons with bleeding disorders requires an in-state doctor to write the prescription. So far, I have not found a doctor in my state who is knowledgeable about the particular genetic mutation that causes me to have a high factor level yet bleed severely. I am now a woman without a treatment center and without treatment.
My chronic pain and suffering affects not only me, but my family as well. Because of my health, we are not living our best life. In spite of this, I am grateful for my experiences, to my sons born with hemophilia, and to Anthony who didn’t survive due to the lack of knowledge that prevails to this very day. This lack prevents his mother from treatment and medication.
I am grateful to Nicholas, who bears witness to the stark contrast of gender care in hemophilia. I have built a career advocating for those like me who are unable to access the care we know is needed. I am appreciative for all of these experiences, but I would also like to be grateful for access to treatment for all women with hemophilia. It is my hope this will be a reality soon.
TIMELINE HIGHLIGHTING A FEW SYMPTOMS THROUGH THE YEARS:
Age 4: my first memory of severe pain in my knees. I had no words to describe the pain and it went unattended.
Age 9: moved to a home in a hilly area. I had pain that brought tears and immobility. Diagnosed with pre-patellar chondromalacia and was instructed to avoid hills and stairs, and to rest, ice and elevate. The constant pain kept me sedentary.
Age 10: my menstrual cycle began with extreme pain, heavy clots, bruises under my eyes and sheer exhaustion. Soaked through sanitary pads and ruined sheets. At school, it seemed I was in the bathroom more than in class. Treatment for this would never come. I spent my menstruating years suffering the effects of anemia.
Age 15: cut my ankle on a jagged piece of wood. The wound kept oozing and reopening, taking a year to fully heal.
Age 16: worked long shifts standing on a hard restaurant floor, in constant pain, fatigued, with swollen knees and ankles. When sitting, I would draw my legs up under my body to prevent my ankles from dangling as the pain was unbearable. Tired and hurting all the time. By the time I became sexually active, I bled with intercourse regardless of my cycle.
Age 21: diagnosed with gout in my toe. I now recognize this was a bleed.
Age 25+: with each of my first 3 pregnancies, I experienced anemia, 2nd trimester spotting, petechial hemorrhaging around my face during childbirth and prolonged postpartum bleeding. 2nd pregnancy brought throbbing pain behind my left eye leading to a spinal tap that would not clot causing a week-long leak of cerebrospinal fluid. 3rd pregnancy resulted in prolonged healing of c-section incision.
Age 27: wisdom teeth extraction bled for weeks.
Age 28: at the ER with excruciating knee pain. Was told there was nothing to be done.
Age 32: sons Anthony and Nicholas were born via C-section. A bleed at the incision caused excruciating pain; bleeding and severe bruising in my groin and down my legs.
Age 35: diagnosed with fibromyalgia.
Age 45: diagnosed with tendinosis (Related to connective tissue disorder).
Age 53: finally diagnosed as a symptomatic carrier of hemophilia A and connective tissue disorder reaffirmed. Was prescribed factor, Amicar® and physical therapy.
Age 56: free factor trials end; I no longer have access to treatment.
Stay informed on the latest trends in healthcare and specialty pharmacy.
Sign up for our monthly e-newsletter, BioMatrix Abstract.
By giving us your contact information and signing up to receive this content, you'll also be receiving marketing materials by email. You can unsubscribe at any time. We value your privacy. Our mailing list is private and will never be sold or shared with a third party. Review our Privacy Policy here.