Sixty percent of adults in the U.S. are living with at least one chronic illness. Forty percent of adults have two or more chronic health conditions.1
Specialty drugs are often prescribed for people with complex and/or chronic medical condition(s). Because many of these conditions can be life-altering and/or threatening, proper support throughout the patient journey is critical for optimal health outcomes. This article provides five benefits for using a specialty pharmacy to help manage chronic or complex medical conditions.
1. Access to Specialty Medication
Due to the complexity of specialty medications and the unique situations faced by the patients who require them for treatment, many specialty drugs are not found at local walk-in retail pharmacies. These medications often require unique patient education tools, patient financial assistance programs, specialized monitoring, advanced packaging, and the ability to get the drug to the patient when and where they need it despite unforeseen events. BioMatrix has met these obligations to our patients for decades.
Specialty pharmacies ensure patients understand their specialty medication insurance coverage, how to get medication in a timely manner, and what financial support options are available. From therapy initiation, payer outreach, benefit investigation, prior authorization, appeals management, and connectivity to manufacturer patient access services, specialty pharmacies coordinate care between all healthcare providers to help patients promptly begin and maintain access to their medication. Our job is to help patients obtain and maintain access to prescribed therapy. We also make sure patients understand how to properly store medications, how to take it, and who to contact when you have questions.
2. Better Adherence and Treatment Outcomes
We know chronic health conditions can complicate daily life. Treatment is often complex, time consuming, expensive, and comes with side effects further complicating things. For all these reasons, up to 50% of chronically ill patients do not take their medication as prescribed.2 By working together, we help make taking your medication easier. Studies show patients who use specialty pharmacies have higher treatment adherence compared to those using a retail option.3 Our data proves this claim. Over the course of one year, BioMatrix conducted a study of patient reported outcomes. Our research found participating patients had an adherence rate of 96.2%. The study showed our services helped to improve both adherence and quality of life. Download the case study here.
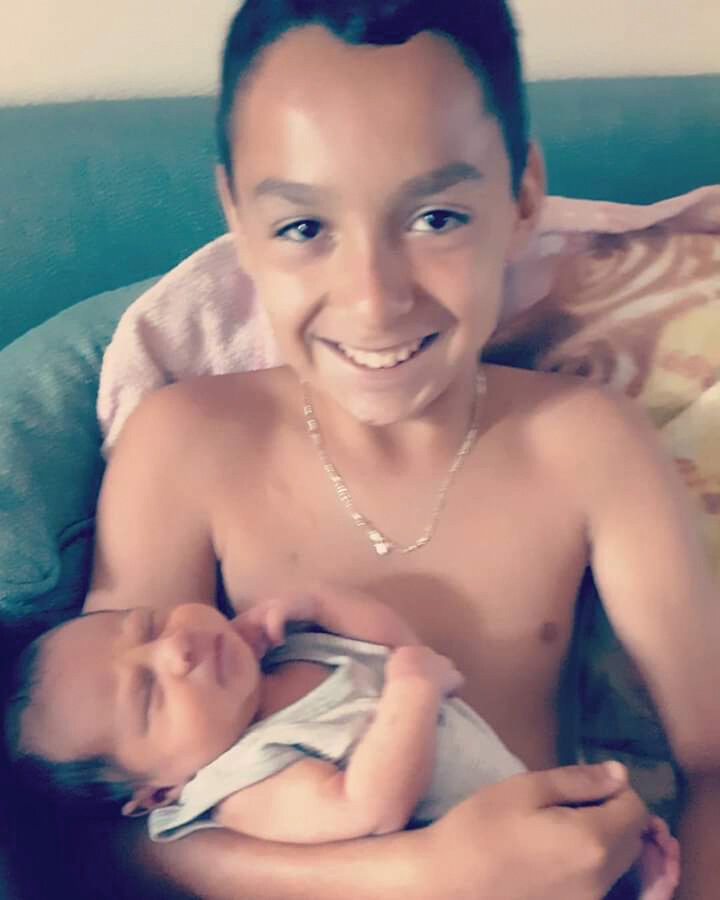
3. In-home Treatment
Due to cost, convenience, and COVID-19, more patients and their providers are opting for home-based treatment. Up to 80% of patients with cancer now receive care in the outpatient setting4 while a new healthcare model set to go into effect April 2021 will provide payment incentives to encourage at-home dialysis. Specialty pharmacists play an important role in helping to manage and monitor treatment in the home environment. We educate patients on what to expect from their prescribed medication and how to properly store, handle, and administer their specialty drugs. Our therapeutically-focused clinical assessments collect and analyze key data while allowing our team to monitor side-effects, medication adherence, barriers to care, and overall response to therapy. Learn how patients at BioMatrix use digital tools to submit refill requests and participate in secure, one-on-one conversations with pharmacy staff from the comfort of their home: click here.
4. Reduced Cost
Living with a chronic condition is costly. When patients have to pay high out-of-pocket costs for their treatment, they’re more likely to skip optional care and delay critical care. This leads to both poorer treatment outcomes and overall health. Poor health can lead to lost workdays and potential loss of employment.5 Research shows6 specialty pharmacies drive down the cost of care in a variety of ways by promoting adherence to therapy, identifying utilization or dosing mistakes, helping to avoid unnecessary hospitalizations, and connecting patients with financial support programs.
BioMatrix is committed to helping patients identify and obtain financial support so treatment can begin without delay. We help identify co-pay assistance programs and connect patients with the right resources for enrollment. From manufacturer co-pay programs to charity-based financial assistance, we provide resources and support helping patients access specialized healthcare without breaking the bank.
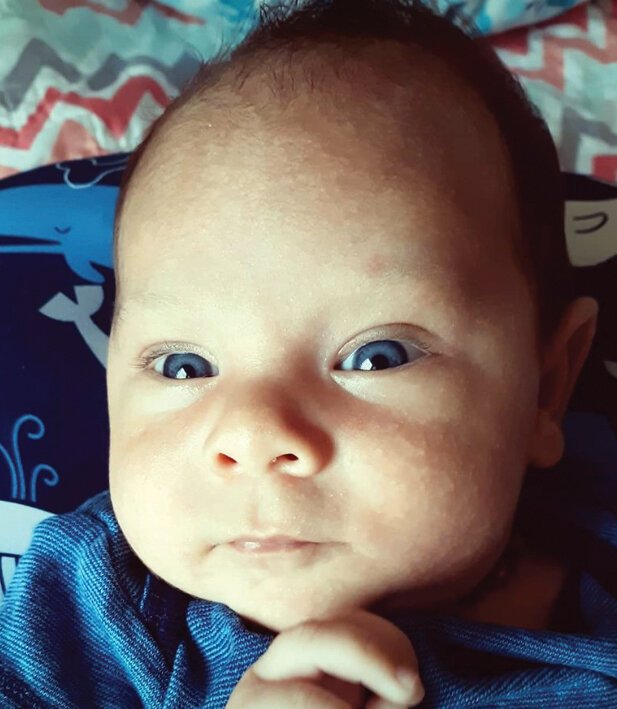
5. Patient-centric Care
A strong relationship between a patient and their health care provider can positively affect the patient’s ability to cope, especially in an outpatient setting.7 In a large study, patients who perceived their health care providers as “knowing them as a person” had higher rates of treatment adherence, more positive beliefs about the effectiveness of their therapy, fewer missed doctor appointments, and a higher quality of life.8 Pharmacists who take the time with each patient to understand needs, challenges, and preferences are better positioned to support, educate, and serve.
BioMatrix Specialty Pharmacy is proud to make a difference in the communities we serve, one patient at a time.
Our clinicians and support staff offer a tailored approach to every therapeutic category, improving quality of life for patients and producing positive outcomes along the healthcare continuum. Learn more.
References
Centers for Disease Control and Prevention (CDC). 2019. Chronic Diseases in America. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
Kleinsinger F. (2018). The unmet challenge of medication nonadherence. The Permanente journal, 22, 18–033. https://doi.org/10.7812/TPP/18-033
Kale HP, Patel AM, Carroll NV. (2018). A comparison of pharmacy dispensing channel use and adherence to specialty drugs among Medicare Part D beneficiaries. Journal of Managed Care Specialty Pharmacy. Apr;24(4):317-326. doi: 10.18553/jmcp.2018.24.4.317.
Cancer care migrates to outpatient setting. Journal of Healthcare Contracting. May 2011. Accessed July 17, 2020. http://www.jhconline.com/cancer-care-migrates-to-outpatient-setting-2.html
Partnership to Fight Chronic Disease. (2019). Framework to Address High Cost Burden for People with Serious Chronic Conditions. https://www.fightchronicdisease.org/resources/framework-address-high-cost- burden-people-serious-chronic-conditions
Joo EH, Rha SY, Ahn JB, Kang HY. Economic and patient-reported outcomes of outpatient home- based versus inpatient hospital-based chemotherapy for patients with colorectal cancer. Support Care Cancer. 2010;19(7):971-978. doi:10.1007/s00520-010-0917-7
Prip A, Møller KA, Nielsen DL, Jarden M, Olsen MH, Danielsen AK. The patient-healthcare professional relationship and communication in the oncology outpatient setting: a systematic review. Cancer Nurs. 2018;41(5):E11-E22. doi:10.1097/NCC.0000000000000533
Beach MC, Keruly J, Moore RD. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J Gen Intern Med. 2006;21(6):661-665. doi:10.1111/j.1525-1497.2006.00399.x
Our entire team is committed to maintaining the health and wellbeing of those we are privileged to serve.
For updated information regarding our response to developments related to COVID-19, a letter from our CEO, and early refill requests, please click here.
Stay healthy, and be well.
We are with you and will get through this together.
Stay informed on the latest trends in healthcare and specialty pharmacy.
Sign up for our monthly e-newsletter, BioMatrix Abstract.
We value your privacy. Review our Privacy Policy here.